Vitamin D, often celebrated for its role in bone health, is now emerging as a key player in the realm of neurological and neurodegenerative health. Recent studies have delved into its potential therapeutic benefits across a spectrum of conditions, including Alzheimer's disease, Parkinson's disease, Huntington's disease, depression, and stroke. Furthermore, the impact of Vitamin D on menopausal women's health has become a topic of significant interest.
Pioneering researchers such as Pragya Komal, Manjari SKV, Sharon Mariam Abraham, Omalur Eshwari, Kishore Golla, Priya Jhelum and Shuvadeep Maity are at the forefront of this exploration. Their work highlights the neuroprotective roles of Vitamin D, examining its anti-apoptotic activities and effects on various disease models. By investigating the molecular mechanisms of Vitamin D, including its influence on gene expression, protein levels, and signaling pathways, these studies provide crucial insights into how this vitamin could potentially serve as a therapeutic agent.
Key points
- Effects of Vitamin D supplementation on neuroprotective roles, anti-apoptotic activities, and its impact on different disease models.
- Research highlights the molecular mechanisms of Vitamin D action, including its effects on gene expression, protein levels, and signaling pathways.
- Various dosages and administration methods of Vitamin D are investigated in different disease models to understand its potential therapeutic benefits.
Research has shown that a lack of vitamin D can lead to impaired neurocognitive performance as well as an increase in the death and loss of neurons. The existing link between vitamin D insufficiency and neuronal dysfunction raises the possibility that VD intervention, when started at the right timing and dosage, could offer therapeutic benefits for a wide range of neuropathological disorders.
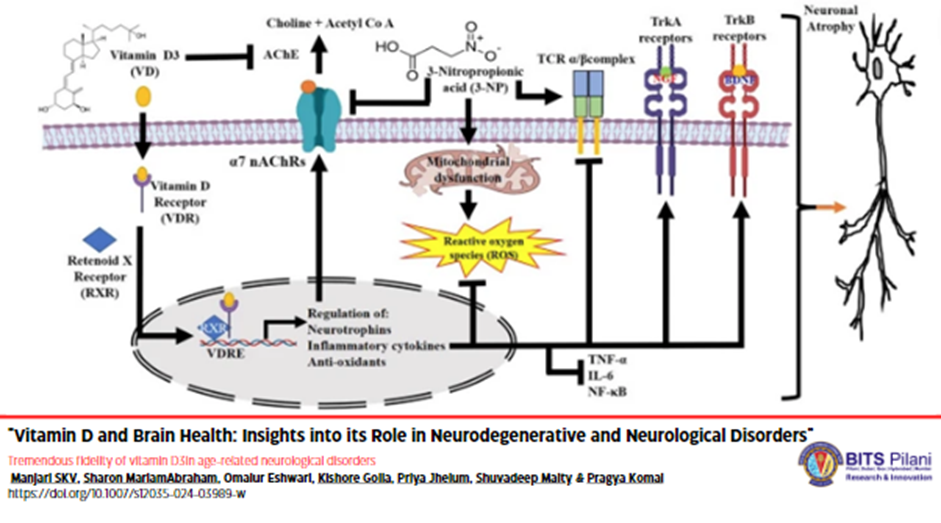
Vitamin D3 (VD) is a secosteroid hormone that exhibits pleotropic effects on brain-related illnesses. It regulates redox imbalance, inflammation, apoptosis, energy production, and growth factor synthesis. Vitamin D3 (VD) is also essential for growth factor development. The active metabolic form of vitamin D3 is called calcitriol or 1,25-dihydroxy vitamin D3 (1,25(OH)2D3). It controls many genes that are involved in neuroinflammation, neuroplasticity, neuroprotection, and neurotropism. According to the findings of a number of studies, a lack of vitamin D may be considered a potential risk factor for the development of several neurological illnesses that are associated with aging. The information shows that having low levels of 25-hydroxyvitamin D3 (25(OH)D3 or calcidiol), which is the main type of vitamin D in the blood, is linked to a higher risk of Alzheimer's disease (AD), Parkinson's disease (PD), Huntington's disease (HD), dementia, and cognitive impairment. Even though there has been evidence for decades that low VD is associated with neurological problems, the particular biochemical mechanism that is responsible for its beneficial effect is still a matter of debate. In our lab, we investigate the neurobiological significance of VD and its benefits in treating various neuropsychiatric illnesses. Since Alzheimer's disease, Parkinson's disease, and Huntington's disease share some clinical, pathological, and epidemiological characteristics, the focus will be on the pathological and epidemiological characteristics of these three diseases. The primary emphasis will be on the various characteristics of VD, including its anti-oxidative, anti-inflammatory, anti-apoptotic, anti-cholinesterase activity, and psychotropic effect within the context of various neurodegenerative illnesses.
Neuronal atrophy is caused by many things, including oxidative stress, neuroinflammation, excitotoxicity, mitochondrial dysfunction, endoplasmic reticulum stress, iron imbalance, and differences in neurotransmitter levels. These problems happen in people with depression, dementia, ALS, MS, AD, PD, and HD. The symptomatic nature of most treatment therapies for these aging-related neurological problems can lead to numerous side effects, including sleepiness, sleeplessness, and anxiety. The consistent use of micronutrients, such as vitamin D3 (VD), may represent a novel strategy. It appears that there may be time- and dose-dependent benefits to taking neurosteroid VD supplements regularly. These benefits may manifest as sex-specific improvements in brain-related disorders and other health issues experienced by aging adults, particularly postmenopausal women. A large-scale study in older women found that VD significantly reduced depression by influencing the dopaminergic system. Researchers think that not getting enough vitamin D might accelerate the aging process and be a major cause of the cognitive, memory, mobility, and motor problems seen in older people worldwide with neurological diseases. Numerous studies in the neuroscience field have demonstrated the positive effects of this inexpensive and readily available nutraceutical on aging and neuropsychiatric disorders.
Therapeutic intervention and consistent consumption of VD beginning in infancy can slow or reverse the neuronal shrinkage that is a hallmark of many mental diseases. Clinical trials including humans with AD, PD, and HD, as well as interventional investigations in animal models of these diseases, provide credence to the current idea. Regular evaluation of calcidiol levels in the brain and serum is necessary to avoid overstating the neurobiological significance of VD. We can adjust the VD dosage based on serum calcidiol levels through dietary changes or external supplementation. We expect factors like gender, race/ethnicity, demographic location, nutrition, and sun exposure to influence the efficacy of visual deprivation interventions on brain health. The current situation calls for immediate agreement on an optimal daily dosage of VD to mitigate the effects of age-related neurodegeneration.


 An Institute of Eminence
An Institute of Eminence